Consider a Career with Transform Rehabilitation! From part-time positions to sign-on bonuses, we could be exactly what you’re looking for!
Available PositionsLegislative Update
January 2021 Update
MEDICARE PHYSICIAN FEE SCHEDULE FINAL RULE
CMS released the 2021 Medicare Physician Fee Schedule final rule on December 1, 2020 which, despite pressure from healthcare providers and members of Congress, included a 10.2% decrease from the 2020 conversion factor. In addition, CMS finalized adjustments to the RVUs for several CPT codes commonly used by therapy providers including:
- Increased work and practice expense RVUs for physical therapy evaluations (97161 – 97163).
- Increased work RVUs and decreased practice expense values for occupational therapy evaluations (97165 – 97167).
- Increased practice expense RVUs for neuromuscular reeducation (97112) and therapeutic activities (97530).
CMS also made adjustments to several work, practice expense, and malpractice GPCIs. Taking into consideration the adjustments to the conversion factor and RVUs, the overall impact to therapy providers was estimated to be roughly -9%, depending on the discipline (PT/OT), locality, and ratio of therapy evaluations to procedure codes.
On December 21st, Congress passed legislation which reduced, but did not entirely eliminate, the scheduled cuts. In addition to the fee schedule adjustments, the legislation also extended the temporary suspension of the Medicare sequestration through March 31st, 2021 and extended the Work Geographic Index floor minimum of 1.000 until January 1st, 2024. CMS published the revised 2021 conversion factor (34.8931) as well as the updated RVU and GPCI files the week of January 4th. The final impact to therapy providers for 2021 has been estimated to be roughly -3.0% depending on the locality and billing practices of the provider, a considerable decrease from the -9% reduction originally included in the final rule.
Additional highlights from the 2021 MPFS Final Rule
- CMS finalized their proposal to have several CPT codes remain temporarily on the Medicare telehealth list through the end of the year in which the PHE for COVID-19 ends. These Category 3 services include:
97161 – 97168, 97110, 97112, 97116, 97535, 97750, 97755, 97760, 97761.
As a result, PTs, PTAs, OTs, and OTAs can provide outpatient therapy services delivered via telehealth and have those services reimbursed by the Medicare program during the PHE. However, despite the addition of these codes to the telehealth list on a Category 3 basis, PTs, OTs, PTAs, and OTAs will NOT be eligible to furnish and bill for telehealth services through the end of a calendar year should the PHE end before then. Even with these codes added to this list on a temporary basis, during the time between the end of the PHE and the remainder of the calendar year in which the PHE ends, telehealth services can only be furnished by a therapist if billed incident to the professional services of a physician or practitioner who is authorized to furnish and bill for telehealth services, provided that the “incident to” requirements are met. - CMS finalized their proposal to allow direct supervision of an assistant by a therapist to be provided using real-time, interactive audio and video technology through the later of the end of the calendar year in which the PHE ends or December 31, 2021. The requirement could be met by the supervising therapist being immediately available to engage via audio/video technology (excluding audio-only) and would not require real-time presence or observation of the service via interactive audio and video technology throughout the performance of the procedure. This provision will allow a PTA or OTA to treat a Medicare Part B beneficiary in a private practice setting without the PT or OT onsite to provide direct supervision. The therapist would just need to be available via audio/video technology.
- The final rule makes permanent CMS’s Part B policy for maintenance therapy services that was adopted on an interim basis for the PHE which allows a physical or occupational therapist the discretion to delegate the performance of maintenance therapy services to a physical therapist assistant or an occupational therapy assistant, as clinically appropriate.
- CMS clarified that therapy students can document in the medical record so long as it is reviewed and verified (signed and dated) by the billing therapist.
- CMS also clarified that the broad policy principle allowing billing clinicians to review and verify documentation added to the medical record for their services by other members of the medical team also applies to therapists.
- The final rule includes several MIPS updates relevant to therapy providers including:
- A performance threshold of 60 points for the 2021 Performance Period
- Reweighting of the Promoting Interoperability and Cost performance categories for physical therapists, occupational therapists and speech-language pathologists for Performance Year 2021. Quality will again account for 85% of the overall MIPS score while Improvement Activities will account for 15%.
- Several measure updates relevant to physical and occupational therapists:
- Measure 226 is now available for reporting by PTs for encounters that include a PT evaluation.
- Measure 128 for registry reporting has been updated to include a new denominator exception code: G2181 – BMI not documented due to medical reason or patient refusal of height or weight measurement.
- Measure 130 for registry reporting has an updated description for the G8430 denominator exception.
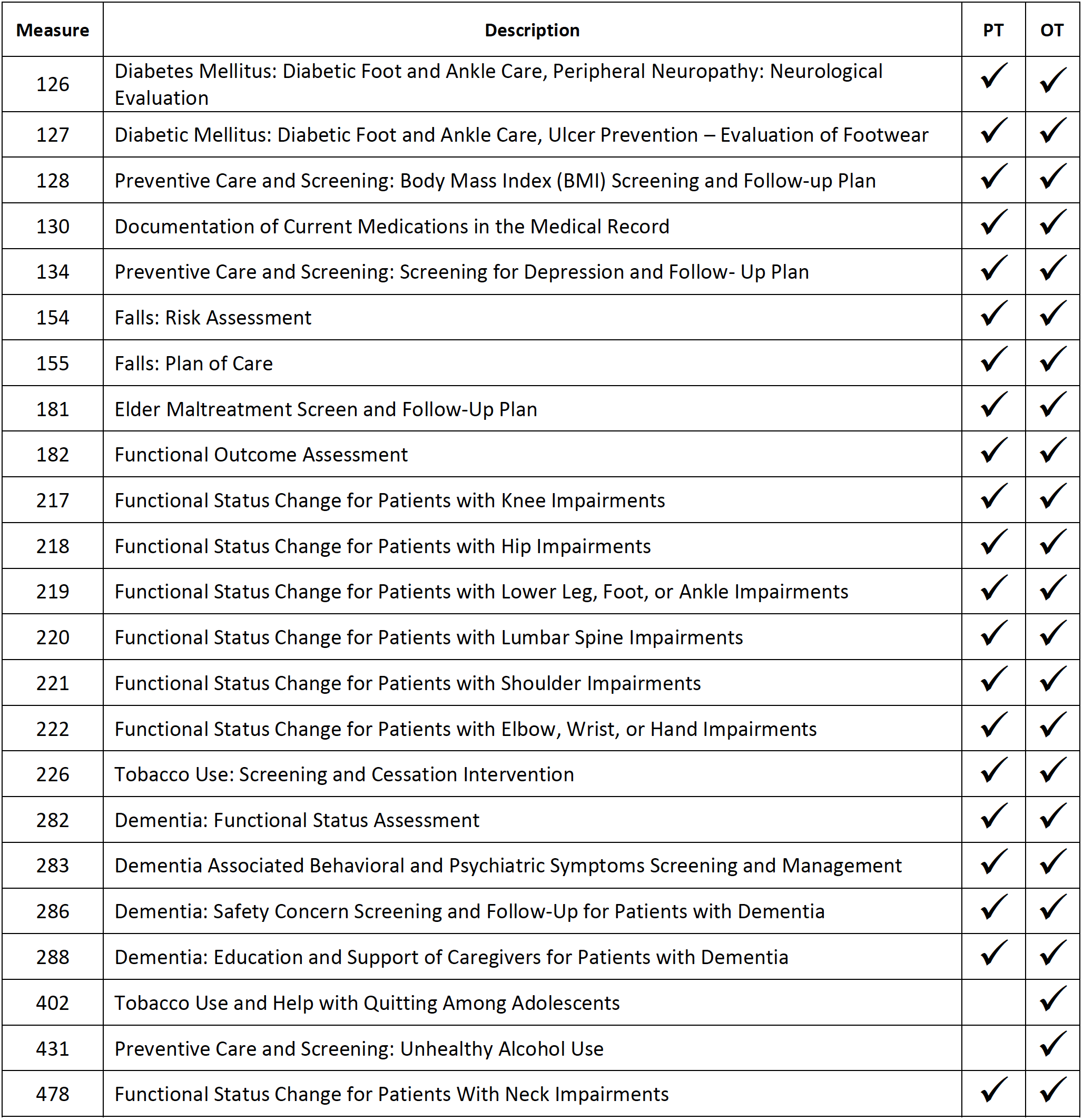
- A full list of Quality measures that are applicable to PTs and OTs is included in the appendix below.
- While not originally included in the final rule, CMS did subsequently publish the KX modifier threshold levels for 2021. The annual threshold levels are $2,110 for PT and speech therapy combined and $2,110 for occupational therapy. The manual medical review threshold remains at $3,000.
NCCI EDITS
Over the course of the past year, CMS has implemented several additions, deletions, and reversals to the CCI edit list that have had an impact on therapy providers. Thankfully, the most recent changes that are effective as of 1/1/21 include some welcome deletions of code pair edits that have historically created reimbursement and denial issues, especially with commercial payors.
Of particular interest to therapy providers is the deletion of the edit for the 97140/97530 pairing as well as the deletion of the edits for 97140 when billed with any eval code (97161, 97162, 97163, 97165, 97166, and 97167). In addition, many of the edits associated with the re-evaluation codes (97164 and 97168) have been deleted including pairings with commonly used codes 97110, 97112, 97113, 97116, 97140, 97150, and 97530. However, not all of the edits associated with the re-evaluation codes were deleted. The -59 modifier will still need to be applied when re-evaluation codes are billed on the same date of service as several modality, wound care, and orthotic management codes.
IRG has once again updated its “-59 Modifier Quick Reference Guide” and distributed it to all clinics to assist clinicians as they navigate the latest round of edit updates. Providers can view the full list of CCI edits here.
PT COMPACT
Twenty states are currently issuing and accepting physical therapy compact privileges including Arizona, Arkansas, Colorado, Iowa, Kentucky, Louisiana, Mississippi, Missouri, Nebraska, New Hampshire, North Carolina, North Dakota, Oklahoma, Oregon, Tennessee, Texas, Utah, Virginia, Washington, and West Virginia.
Another nine states have enacted compact legislation but have yet to begin issuing or accepting compact privileges including Delaware, Georgia, Maryland, Montana, New Jersey, Pennsylvania, South Carolina, South Dakota, and Wisconsin.
APPENDIX
Applicable 2021 Registry Quality Measures for PTs and OTs
December 2020 Update
As the year comes to a close, therapy providers are looking ahead to 2021 and the impending reimbursement cuts that are scheduled to take effect on January 1st. Fortunately, Congress has been working to stop these cuts from taking effect. Through its affiliation with the Alliance for Physical Therapy Quality and Innovation (APTQI), Upstream has committed resources to lobbying and advocacy efforts to help fight these cuts. In addition, Upstream continues to stay abreast of legislative developments that would have a significant impact on therapy providers if passed. A quick summary of several pieces of legislation of interest which Upstream will continue to monitor in the coming weeks and months:
H.R. 8702 (“Holding Providers Harmless From Medicare Cuts During COVID-19 Act OF 2020”)
On October 30th, Reps. Ami Bera (D-CA) and Larry Bucshon (R-IN) introduced legislation (H.R. 8702) in the House of Representatives which would add funding to Medicare and direct CMS to essentially reset payment to 2020 levels for providers facing reimbursement cuts. Known as the “Holding Providers Harmless From Medicare Cuts During COVID-19 Act of 2020”, this bipartisan legislation would enable pay increases for primary care and other providers who often provide E/M services, while avoiding devastating, corresponding cuts for millions of other providers due to Medicare’s budget neutrality requirements. If passed, the legislation would effectively freeze payments at 2020 rates for services scheduled to be cut in 2021 for a period of two years while allowing the planned E/M increases to take place as scheduled. In a nutshell, if a code billed in 2021 carried a higher reimbursement in 2020, the provider would be still be paid at the lower rate established for 2021 plus an additional payment in order to level the total payment to the 2020 rate. There has been some concern if the bill were to pass as written that other payers who adopt the Medicare fee schedule would reference the 2021 Conversion Factor and RVUs as finalized but not make similar adjustments to offset the cuts.
H.R. 8505
Earlier in October, Michael Burgess (R-TX) and Bobby Rush (D-IL) introduced H.R. 8505, a bill that would establish a one-year delay of implementation of the cuts, paid for through the Pandemic Provider Relief Fund. If passed, this bipartisan legislation would temporarily waive budget neutrality adjustments under the Medicare Physician Fee Schedule. By waiving Medicare’s budget neutrality rule for one year, the legislation would give the Department of Health and Human Services and CMS the ability to immediately delay or mitigate the proposed cuts while allowing the scheduled payment increases to go into effect for primary care and other physician office visits. While a one-year delay offset by $10b from provider relief funds would not provide a long-term fix, it would allow time for affected specialties to lobby for a permanent consensus plan going forward.
H.R. 7154 (“Outpatient Therapy Modernization and Stabilization Act”)
In June, Reps. Brendan Boyle (D-PA) and Vern Buchanan (R-FL) introduced H.R. 7154, also known as the “Outpatient Therapy Modernization and Stabilization Act” in the House. The bill targets the proposed 2021 reimbursement cuts as well as several other key issues relevant to the therapy profession. In regard to the cuts, the bill would provide a one-year budget neutrality exemption so that payment increases for other providers do not force payment cuts for other specialties. In addition, the legislation includes an amendment to the telehealth provisions of the Medicare statute that would permanently allow physical, occupational, and speech therapy providers to bill for services furnished via telehealth as well as adjustments to the Medicare Physician Fee Schedule that would result in payment increases of 1% in 2021 and 0.5% in 2022 and 2023. The bill would also reduce administrative burdens by clarifying that either a physician’s signed order/referral for therapy services OR a signed plan of care would satisfy certification requirements but not both, as is currently the case.
H.R. 8755 (“Expanded Telehealth Access Act”)
Reps. Mikie Sherrill (D-NJ) and David McKinley (R-WV) introduced the Expanded Telehealth Access Act (H.R. 8755) in the House on November 16th, 2020. The bill proposes to add physical, occupational, and speech therapists to the list of providers that are eligible to provide telehealth services to Medicare beneficiaries. CMS has indicated that it does not have the authority to extend the current telehealth therapy provisions under the PHE without Congressional action. This legislation would make permanent the reimbursement eligibility for PTs, OTs, and SLPs and permits the Secretary of the Department of Health and Human Services to expand this list. While the proposed legislation may face challenges as a stand-alone bill, there is hope that several similar bills could be grouped in a bipartisan package and/or possibly included in a future stimulus package.